- Date:2023-10-23
- Click:5442Times
Do you often come across such people around you: frequent recurrent migraine headaches, very much affecting learning and work, and in serious cases, you can only rest in bed; many unexplained cerebral infarction episodes; in order to cure this annoying migraine headache, unexplained cerebral infarction, spent all the family's lifelong savings, and did a lot of tests but did not find the problem. At this time, you may want to let the right heart acoustic imaging test help you find the cause of the disease.
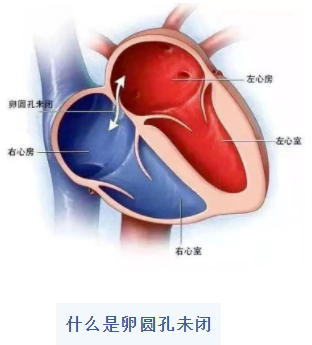
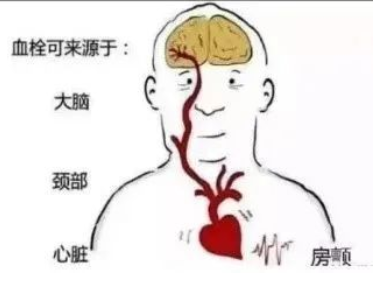
Right heart acoustic imaging mainly screens for patent foramen ovale, which usually closes within the first year of life. If the foramen ovale does not close by the age of 3 years or older, it is called patent foramen ovale (PFO), which has an incidence of about 25% in the population and is the most common anatomical abnormality of the heart. PFO is the most common anatomical abnormality of the heart. When the patient's right atrial pressure is elevated by various causes (e.g., strenuous exercise, coughing, diving, etc.), the patent foramen ovale can develop an abnormal right-to-left shunt when it exceeds that of the left atrium. Venous blood (low in oxygen) mixed with arterial blood and paradoxical embolism can cause vascular clinical syndromes such as stroke, migraine, decompression sickness, and reclining respiratory-oblique hypoxemia. Patients may present with clinical manifestations such as headache, dizziness, dyspnea, or limb weakness.
Some studies have shown that the detection rate of patent foramen ovale is three times higher in migraineurs than in the healthy population. Ovoid foramen undulant plays an important role in the mechanism of migraine cerebral infarction.
What is right heart acoustic imaging?
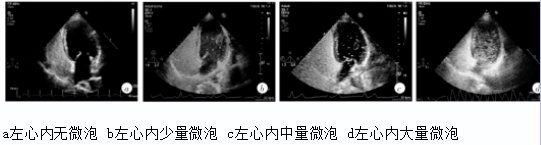
The main principle is to utilize the huge acoustic impedance difference between the microbubbles and the blood, so that a strong reflection occurs. The diameter of human lung capillaries is 6~9μm, while the diameter of microbubbles of the right heart acoustic contrast agent is >10μm, so the microbubbles injected intravenously can't enter into the left heart through the pulmonary circulation, and can only be visualized in the right heart, so it is called the right heart acoustic contrast.
If the operator detects the signal of microbubbles in the left heart, it means that there is an abnormal channel in the heart chambers or outside the heart.
How is right heart acoustic imaging performed?
Many people are already afraid of the word “imaging”, but it is actually just an indwelling needle. Right heart acoustic imaging is a non-invasive, non-radiation, easy and economical imaging technique.
By injecting contrast agent (oscillating sterile saline) through a peripheral elbow vein and combining it with cardiac ultrasonography, the anatomy and blood flow of the right heart system can be understood, helping to determine the cause of the disease. Moreover, the right heart acoustic contrast examination is short, and the patient can complete the examination in a more comfortable state. The Department of Cardiac Ultrasound at our hospital is now mature enough to carry out this technique.
Who should consider right heart acoustic imaging?
1. patients with migraine, especially those with migraine with aura (with recurrent episodes of visual abnormalities);
2. patients with ischemic stroke of unknown cause, transient ischemic attack, and asymptomatic cerebral infarction;
3. patients with unexplained syncope;
4. cardiac diseases suspected to have left-to-right or right-to-left shunts, such as screening for patent foramen ovale, patent foramen ovale blockage, atrial septal defects and ventricular septal defects, and the presence or absence of residual shunts after blockage;
5. suspicion of congenital vascular malformations such as permanent left superior vena cava and pulmonary arteriovenous fistulae
6. to assess the internal diameter of the right heart chambers, the contour of the endocardial border, the thickness of the ventricular wall, the presence of occupancy, and the presence of valvular regurgitation
7. to find the etiology for patients with hypoxemia.


 鲁ICP备11009722号-4
鲁ICP备11009722号-4 